Understanding Diabetic Retinopathy
As people who live with a chronic illness like type 1 diabetes, we are repeatedly made aware of the complications that can arise as a result of uncontrolled blood sugars for extended periods. Take a second to recollect your initial interactions with the endocrinologists? Featuring somewhere in the discussion would be the effect of unmanaged BG on your eyes and vision. High blood glucose levels tend to affect our blood vessels. The blood vessels in our kidneys and eyes are the more fragile and thus tend to be affected the most with long periods of high and uncontrolled BG levels.
This condition is called Diabetic Retinopathy. I reached out to my ophthalmologist for getting deeper insights to sum up retinopathy for you.
So what exactly is Diabetic Retinopathy?
Diabetic Retinopathy is a medical condition where the retina gets affected and hence the name “Diabetic Retinopathy”
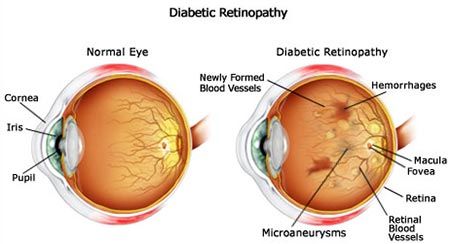
In the human eye, retina is the light-sensitive innermost layer of the eye. The retina acts like the film of a camera and sends the images to the brain for it to process so that we can see everything around us clearly.
Diabetic retinopathy can lead to blindness if not managed properly. Blindness caused by diabetic retinopathy can be easily avoided with a tighter control on your BG levels.
While HBA1C is considered as your reference point for assessing your controls, it’s now proven that “time in range” is a better yardstick to measure your controls. Irrespective of what reference points for the controls you keep, the bottom line is, the ONLY way to avoid developing retinopathy is keeping tight control on your BG levels (whilst remaining sane in the process!)
Causes
Simply put, uncontrolled BG levels for a long period of time damage the blood vessels and lead to retinopathy. The blood vessels in the retina become leaky or get blocked due to consistently high BG levels causing retinopathy.

To put into layman terms, macula is the most important central part of our retina that helps us to see the colours and fine details clearly. Due to retinopathy there is a fluid leak into macula and thus there is blurry vision. Sometimes the blood vessels get blocked causing impaired supply of oxygen and nutrients to the fragile retina. To improve blood circulation in the retina, new blood vessels may form on its surface. But these blood vessels are fragile abnormal blood vessels and can leak blood into the back of the eye causing loss of vision.
While retinopathy is primarily caused due to high BG levels, other medical conditions like high BP, anaemia and high cholesterol levels can also contribute to the development of this disease.
Symptoms
- Seeing spots or floaters
- Blurred vision
- Having a dark or empty spot in the centre of your vision
- Difficulty seeing well at night
Waiting for symptoms to appear before seeking medical attention is not the correct approach and a regular annual screening of the eyes is a must. Do keep an eye on (pun not intended) the above factors to prevent the development of retinopathy.
Diagnosis
Diabetic Retinopathy can be diagnosed by visiting an ophthalmologist who would conduct a comprehensive eye examination. This examination focuses on evaluating the retina and macula.
Diagnostic tests
1. Patient history to determine vision difficulties, presence of diabetes, and other general health concerns that may be affecting vision
2. Visual acuity measurements to determine how much central vision has been affected
3. Refraction to determine if a new eyeglass prescription is needed
4. Evaluation of the ocular structures, including the evaluation of the retina through a dilated pupil
5. Measurement of the pressure within the eye
Supplementary tests may include:
- Retinal photography or tomography to document current status of the retina
- Fluorescein angiography to evaluate abnormal blood vessel growth
Carry these things when you go for a diagnostic test :
- Your BG logbook (manual or through apps and reports). The idea is to give your ophthalmologist a quick glance view of your BG management in the last few weeks / months.
- List of all the medications you are currently taking.
It is advisable to not drive back on your own since your eyes are dilated for the test. Please plan your visit accordingly.

Frequency of tests
The normal protocol says that these tests be conducted annually but there are few other things to be noted. First, detection and onset of diabetes are two different things. So it’s a possibility that the onset of T1D was way before the diagnosis. Hence screening of eyes for retinopathy is insisted upon immediately after diagnosis. If there are no changes in the retina, then the tests can be done annually. In case any changes are observed, the frequency of the tests is increased. The frequency is decided basis the severity of the changes.
Whatever frequency is suitable for you, it would help if you start scheduling these visits in your calendar. That would make sure that you don't miss the appointments.
Stages
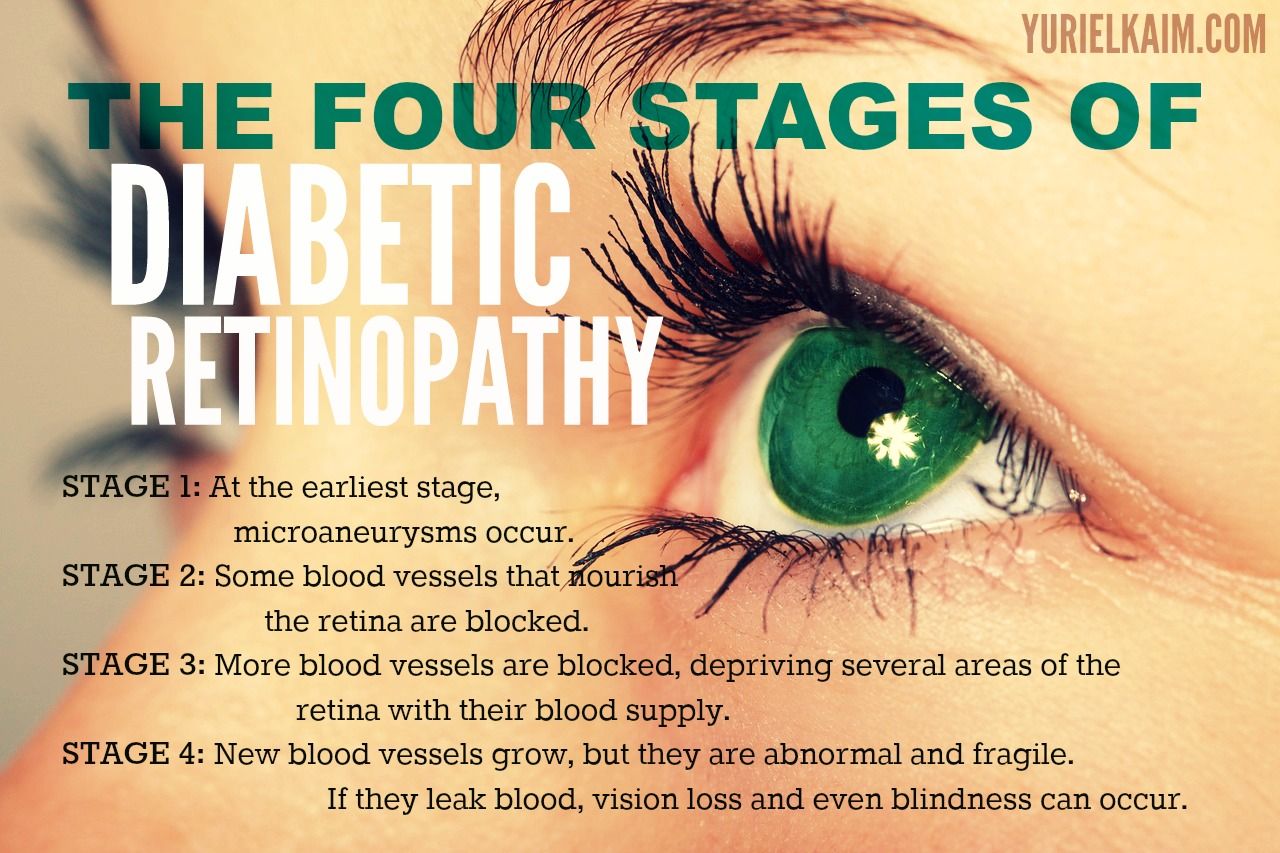
Diabetic Retinopathy has 4 stages
1. Mild Non-proliferative Retinopathy: At this stage, micro aneurysms occur. They are small areas of balloon-like swelling in the retina's tiny blood vessels. The symptoms don’t show much at this stage.
2. Moderate Non-proliferative Retinopathy: This stage is when blood vessels that nourish the retina are blocked.
3. Severe Non-proliferative Retinopathy: In this stage, many more blood vessels are blocked, depriving several areas of the retina with their blood supply. These areas of the retina send signals to the body to grow new blood vessels for nourishment.
4.Proliferative Retinopathy: At this advanced stage, signals sent by the retina for nourishment trigger the growth of new blood vessels. These new blood vessels are abnormal and fragile. They grow along the retina and along the surface of the clear, vitreous gel that fills the inside of the eye. By themselves, these blood vessels do not cause symptoms or vision loss. However, they have thin, fragile walls. If they leak blood, severe vision loss and even blindness can result.
Prevention
You only have one retina and you need it to work effectively throughout your life to be able to see properly. Hence the aim is not to wait for the symptoms to show, but be proactive and try to avoid the development of this disease in the first place.
The following is a list of things you can take note of as a T1D to prevent developing retinopathy
- Avoid smoking and alcohol
- Exercise regularly
- Be mindful of what your meals and in between the meals snacking
- Be regular with your annual diabetic tests where your urine protein, feet, and other checks are carried out
- Try keeping your BP, sugars and fat levels under control.
- Lastly keep getting your eyes checked periodically
They say prevention is better than cure, always! So do your best to prevent developing retinopathy in the first place. These tips are even beneficial in case retinopathy develops and you wish to stop the disease from progressing further.
Is it curable / treatable?
The treatment for diabetic retinopathy depends upon the severity of the damage caused by diabetic retinopathy. The idea behind any such action is to slow the progression of the disease.
In the early stages of non-proliferative diabetic retinopathy, regular monitoring may be the only treatment. Following your doctor's advice for diet and exercise and controlling blood sugar levels can help control the progression of the disease.
If the disease advances, the blood vessels can leak blood and fluid into the retina, leading to macular edema. Earlier laser treatment (photocoagulation) was used to stop this leakage. A laser beam of light creates small burns in areas of the retina with abnormal blood vessels to try to seal the leaks.
But over time, antibodies called bevacizumab and ranibizumab are used alongside laser treatment to treat retinopathy. These were initially made for cancer treatments but have over time worked wonders in the treatment of retinopathy. The only downside to this treatment is that it is invasive in nature and is injected in your eye directly. It doesn’t stay in the eye for very long and requires a repeat process multiple times and hence is risky. However, due to its ability to aid in the treatment of retinopathy, it is widely accepted.
Myths
Myth 1: T1Ds are affected by diabetic retinopathy while T2Ds are 'safe'
Statistically, 20 % of T1D and 25% of T2D are affected by retinopathy at the end of 10 years while at the end of 20 years this percentage is 90% and 60% for T1D and T2D and it’s true that T2D suffer less microvascular complications than other diabetics.
But after 20 years of living with diabetes, irrespective of whether you are a T1D or T2D, almost 95 % of all diabetics with uncontrolled BG develop retinopathy.
Myth 2: Aspirin isn’t good for me!
Studies have shown that the use of aspirin does not worsen diabetic retinopathy. Each patient is different, so consult your doctor before you start an aspirin regimen.
Myth 3: If I can see, my eyes are healthy!
Visual acuity is important, but it doesn’t mean that you’re healthy. The aim of treatment is prevent further loss of vision and waiting for symptoms means that it's already late.
Top tips to avoid and manage retinopathy
- Frequent Screening
We only have one retina throughout our lives and we have to focus on saving it. We can’t wait around for the symptoms to show up before taking proactive actions, hence frequent screening is a mandatory chore for T1Ds.
2. Mange your other medical conditions well
BP, cholesterol etc. need to be managed since these aid the development of this disease.
3. It’s a lifelong process
Don’t assume that if laser treatment or one screening has been done, you are free. Make this a regular affair. Keep at it to ensure longevity of your eye health (and your health as well)
Who is the correct person to visit?
Of course, an ophthalmologist is the correct person to visit besides your endocrinologist.
While I take all precautions to avoid diabetic retinopathy at all costs, our friend, Shekhar Milani who has undergone a dual kidney and pancreas transplant, shared with us his experience of dealing with diabetic retinopathy.
While at work on an ordinary working day in 2014, he suddenly lost his vision in the right eye.
Not sure of what had happened, he called up his sister, asking her to meet at the hospital. He was told he had diabetic retinopathy. There had been severe bleeding in his right eye while the left eye had a very minor bleeding. What intrigued me while Shekhar spoke about his retinopathy was that he didn’t have a single symptom before he landed up in the hospital with vision loss.
As has been said by the ophthalmologist above, the symptoms don’t really show in the early stages of retinopathy, hence timely screening is of utmost importance. He was told that he required immediate surgery. Within a span of 4-5 days, his right eye was operated upon along with laser treatment. He had to take a ton of precautions initially after the surgery. He couldn’t take a head bath for a month and wasn’t allowed to use the phone or TV also. For the left eye, only laser treatment worked well. At the time of surgery he was told that he might regain 30-40% vision in his eyes, but as of today he has 50-60% vision in his eyes. In fact Shekhar told me that post his transplant the vision has gotten even better. We all recently drove down for a holiday on the outskirts of Pune and Shekhar drove the entire time and this was a great thing to see.
Shekhar is no longer a T1D and I asked him after his retinopathy experience what advice he would give to other T1s and he said, discipline with regards to your BG levels, as suggested by the ophthalmologist as well. With that I hope everybody reading this takes their cue to work towards avoiding this diabetic complication.
SUPPORT BLUE CIRCLE DIABETES FOUNDATION
We need your help and support to continue to grow, expand and touch the lives of countless people in the diabetic community. Every little bit helps us in sustaining this endeavour.
Click here to donate