Taking care of your feet with diabetes
Talking about diabetes related complications my endocrinologist always says,
“Diabetes can affect everything from the hair on your head to the toe nail on your foot”. And it’s absolutely true!
When we visit the doctor’s office, we are told to take care of our feet. Research studies have proven that uncontrolled BG over extended periods of time is the leading cause of blindness, kidney failure, heart attacks, stroke, diabetic retinopathy and lower limb amputation.
Prolonged high BG levels can lead to various types of foot issues like :
1. Diabetic Neuropathy
Uncontrolled BG levels can lead to severe nerve damage in the feet. It causes a tingling sensation in the feet and is often quite painful. It also results in a loss of sensation in the foot which could mean that you may not 'feel' your wounds.
2. Gangrene
If sugars are always high, it can lead to a decreased flow of blood to the feet and thus any wound on the feet may not heal (as quick as it should). This could lead to gangrene, which is tissue death due to absence of blood circulation. It can be life threatening if bacterial infection develops (wet gangrene). In severe cases gangrene may lead to amputation.
3. Charcoat Foot
Uncontrolled diabetes can also lead to a change in the shape of the feet. It starts with redness, warmth, and swelling. Later, bones in your feet and toes can shift or break, which can cause your feet to have an odd shape, such as a “rocker bottom.”

4. Various foot problems like ulcers, bunions, corns, calluses, fungal infection, dryness of the skin, and ingrown toenails.
Diabetic neuropathy should be monitored closely since untreated neuropathy could lead to various complications being developed like gangrene, charcoat foot, etc.
Diabetic Neuropathy
While there are many foot problems, nerve damage, also called neuropathy affects majority of the affected people. Diabetic neuropathy is nerve damage caused by prolonged high blood sugars. When it affects the arms, hands, legs and feet, it is known as diabetic peripheral neuropathy.
Diabetic neuropathy impacts three different types of nerves:
- Sensory nerves, which enable us to feel pain, temperature and other sensations
- Motor nerves, which control the muscles and give them their strength and tone
- Autonomic nerves, which allow the body to perform certain involuntary functions, such as sweating
Diabetic peripheral neuropathy develops slowly and worsens over time. It maybe asymptomatic for a very long time before it's diagnosed for the majority. This loss of sensation and other problems associated with nerve damage increases the chances of developing skin ulcers (open sores) that can become infected and healing is more difficult.
Uncontrolled blood sugars for several years increases the likelihood of diabetic neuropathy.
Symptoms
Depending on the type(s) of nerves involved, one or more symptoms may be present in diabetic peripheral neuropathy.
For sensory neuropathy:
- Numbness or tingling in the feet
- Pain or discomfort in the feet or legs, including prickly, sharp pain or burning feet
For motor neuropathy:
- Muscle weakness and loss of muscle tone in the feet and lower legs
- Loss of balance
- Changes in foot shape that can lead to areas of increased pressure
For autonomic neuropathy:
- Dry feet
- Cracked skin
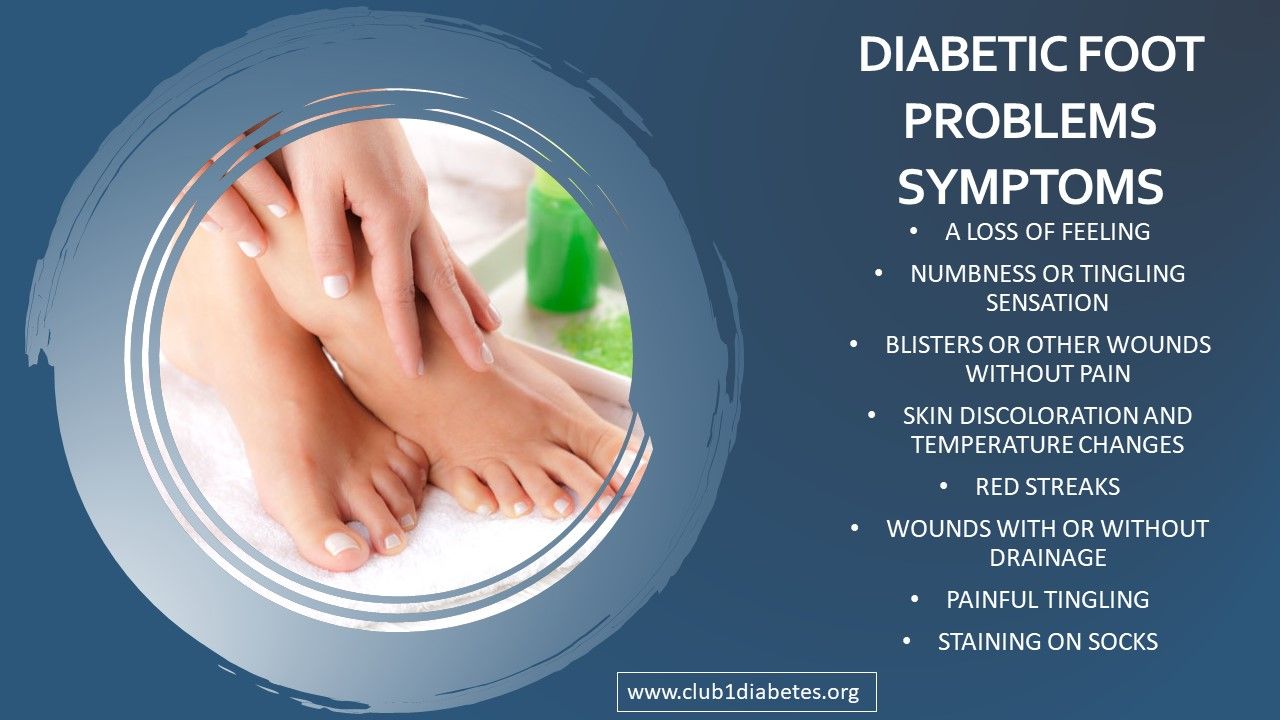
If you feel you display any of the above symptoms, you must act proactively and meet with your doctors and get diagnostic tests done and start treatment as per the recommendation of your doctors.
Diagnosis
Diagnosis of diabetic neuropathy is done by examining the foot and ankle and the examining doctor will obtain the patient’s history of symptoms and will perform simple in-office tests on the feet and legs. This will help in evaluating and assessing the patient’s reflexes, ability to feel light touch and ability to feel vibration. The doctor may refer to additional tests based upon the findings and these tests may vary from case to case.
Treatment
Based upon the diagnosis, doctors could prescribe oral medications or some combination of oral medications. In case the damage is severe, it might need surgery.
It’s important to note that bringing BG under control will help avoid further damage. Prevention is better than cure!
Points to remember
1. Keep your BG in range :
Prevention is better than cure and keeping BG levels in range is a great start point to avoid all complications.
2. Wash and examine feet daily:
Keep feet clean to prevent infections, wash and dry well. Inspect your feet everyday, check soles, between the toes, to look for anything abnormal and bring it to the attention of your doctor if you notice something. If your skin is dry and cracked, lubricate your foot.
3. Avoid walking barefoot:
Protect feet in socks and shoes. Buy and wear comfortable shoes. A podiatrist may recommend special shoes to help prevent deformities. Do not wear socks so tightly that they restrict blood flow. There are many diabetes friendly socks available in the market for those specifically looking such products.
4. Promote blood flow to the feet:
Put feet up when sitting, wiggle your toes periodically, and get enough exercise. These actions help promote healthy blood flow to the feet.
5. Care for corns and bunions:
Treat corns and bunions carefully. Never shave corns, as this increases the risk of infection.
6. Avoid smoking:
Smoking adversely affects blood flow to the tissues, which can make foot problems worse in people with diabetes.
Take care of your feet and let's walk and dance our way through life!
SUPPORT BLUE CIRCLE DIABETES FOUNDATION
We need your help and support to continue to grow, expand and touch the lives of countless people in the diabetic community. Every little bit helps us in sustaining this endeavour.
Click here to donate