Menstruation and diabetes management
Of the scores of things that have an effect on blood sugars such as basal, bolus, food, weather, illness (read the sick day management guide), different types of exercise, stress, among lots others, women with diabetes have one more variable to deal with - menstruation. While I have been a type one diabetic for over two decades, I realized only a few years ago by observing myself and reading up that female hormones have a considerable effect on glycemic variability.
I always believed that my periods had no role to play in my rollercoaster of blood sugars all these years. I couldn't be more wrong. Once I transitioned to the low carb way of eating, the law of small numbers automatically eliminated a ton of variables, making it easier to pin point what factors were really affecting my BG. For a lot of women, low carb has also regulated their cycles (I already had a fairly regular cycle so there wasn't much change there in my case)
As it is, menstruation has been a much ignored and socially unacceptable topic to discuss in the Indian context over the years. It is either considered a time of impurity and exclusion from social or religious gatherings or at the other end of the spectrum, in some cultures it is a time for celebration on account of a young woman's first period. The problematic part in my opinion, is that menstruation is usually not taken for what it is - a biological process. Nothing more, nothing less. Women underplay as well as hesitate to discuss their menstrual health issues openly and a lot of women do not even know the basics of their own anatomy, partly even because of the dismal levels of education and discussions on such topics in schools, which are divided, gendered and far from inclusive. A lot of families are hesitant to talk about these so called 'uncomfortable issues' too.

While these issues may seem distant and not directly related to the cause of the impact of the menstrual cycle on blood sugars, the fact is that as long as we do not talk openly and share our experiences, we would never know if something affects our blood sugars and to what degree.
So here is a quick science lesson on the female menstrual cycle :
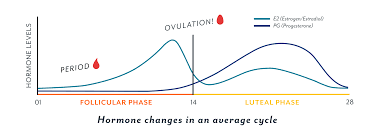
There are three major parts to an average 28 day cycle (cycles could be anywhere between 21-35 days too) and here is how they affect our sugars :
1. Follicular phase - It starts on the first day of the period. It is named so because of the Follicle Stimulating Hormone (FSH) created in the body at that time. If I do not reduce my basals (which had been increased by 25-30%) back to normal by the first two days of my period, I would be correcting hypos throughout the day. Insulin sensitivity increases in the follicular phase.
2. Ovulation phase - It occurs mid cycle, between the follicular phase and the luteal phase, around the 14th day or so on an average. Progesterone levels slowly start increasing once ovulation occurs. For some, a little insulin resistance has begun already and basals might need to be bumped up.
3. Luteal phase - occurs after ovulation and before the follicular phase. This is the phase of highest insulin resistance which occurs in days leading up to the first day of periods and when you might need a higher basal profile.

Here are a few tips on how to stay on top of your blood sugar management with regards to your menstrual cycle :
1. Test BG often
If you are trying to figure out a pattern that needs to be fixed, you need to test often enough for a pattern to emerge in the first place. So just test, test, test whether you use a glucometer, FGM or CGM! There is no upper limit to how many times you can or should test.
2. Tracker
The next logical thing to do after testing BGs often is to log them down so that you can have an overview and co relate stuff. Apart from logging BG, logging your cycle is also important. There are a lot of period tracking apps that can predict cycles available as well that can help you stay on top of the game. Here is a sample of a menstrual journal that you can use to manually write down and track, starting from the first day that bleeding begins to the end of the month.
3. Different basals (Pro tip!)
Having different basal profiles for different times of the month works for a most women, including me. If you are not doing it yet, try it out! With a lot of trial and error (read : spiking and crashing) I have come to the understanding that my body has 25 to 30% higher basal needs right before my periods start. So I hike my basals likewise about 4-5 days or a week prior to the first day of my period and drop them back to normal or sometimes even -10% in the first 2-3 days of my period. Read more about basal testing.
4. Bolus -
Bolus requirements might go up, meaning that for certain times of the month, your ICR (Insulin to Carb Ratio) changes as well and you may need more meal time insulin for the same meals.
5. Metformin -
Extended release metformin is known to stabilize irregular blood sugars during the menstrual cycle. You can talk to your healthcare provider to see if you might need to use it.
Let's get one step closer to getting better blood sugar control, girls!

SUPPORT BLUE CIRCLE DIABETES FOUNDATION
We need your help and support to continue to grow, expand and touch the lives of countless people in the diabetic community. Every little bit helps us in sustaining this endeavour.
Click here to donate